Turn drug delays
into seamless starts
Our AI workers streamline back-office tasks in your EHR, leveraging millions of buy-and-bill datapoints to optimize specialty drug treatment workflows.
Used by organizations processing 100k+ patients a month
Partnered With Companies Like
Redefining Specialty Therapy Administration
Mandolin’s AI-driven automation is transforming how specialty therapies are delivered. Here’s how we make an impact.
90%
Reduced Manual Work
3x
Faster Time-To-Therapy
99%
Task Completion Accuracy
$5bn
In Drugs Enabled To Date
Learn about our workflow
No APIs. No integrations. Every step, fully automated.
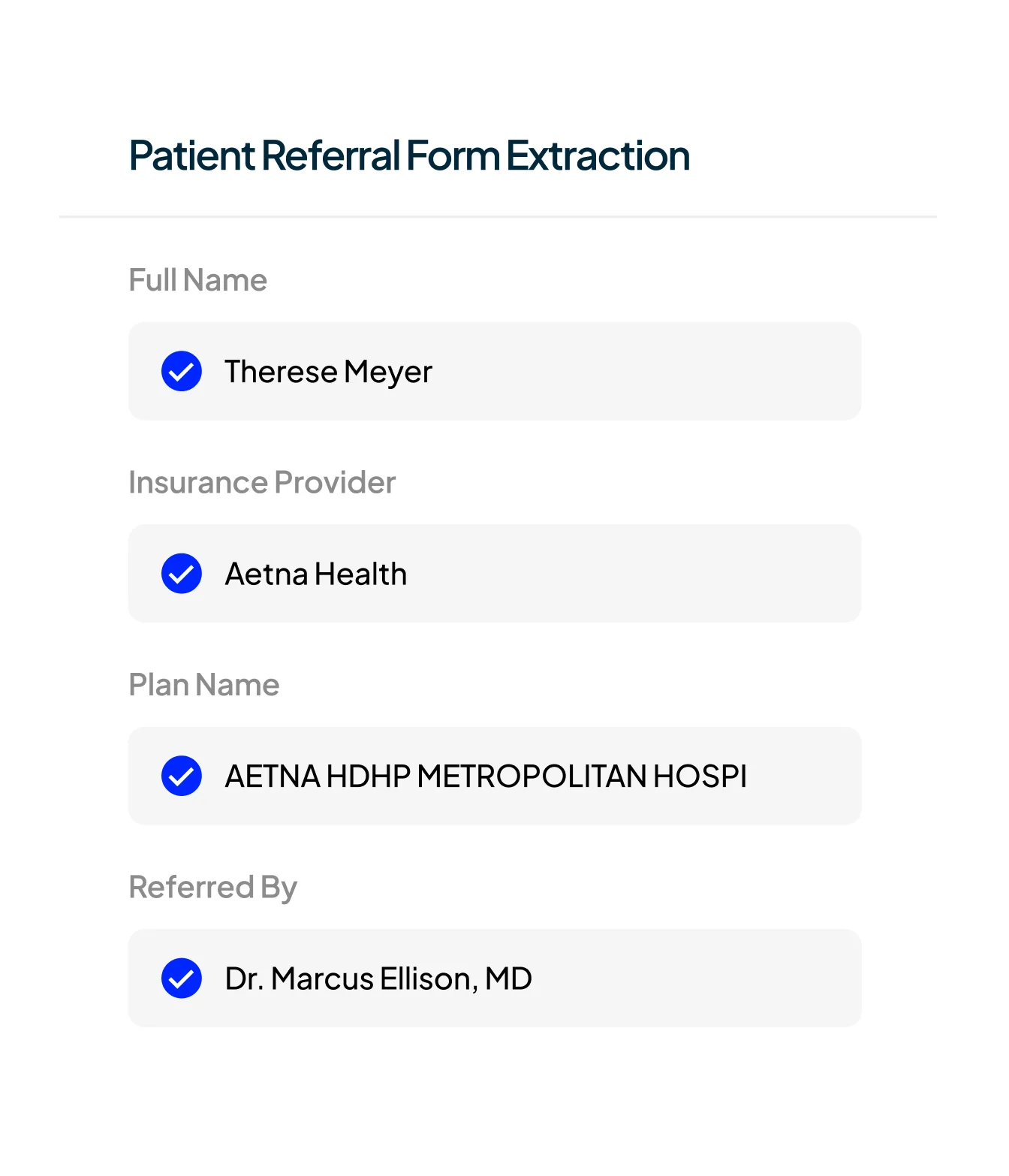
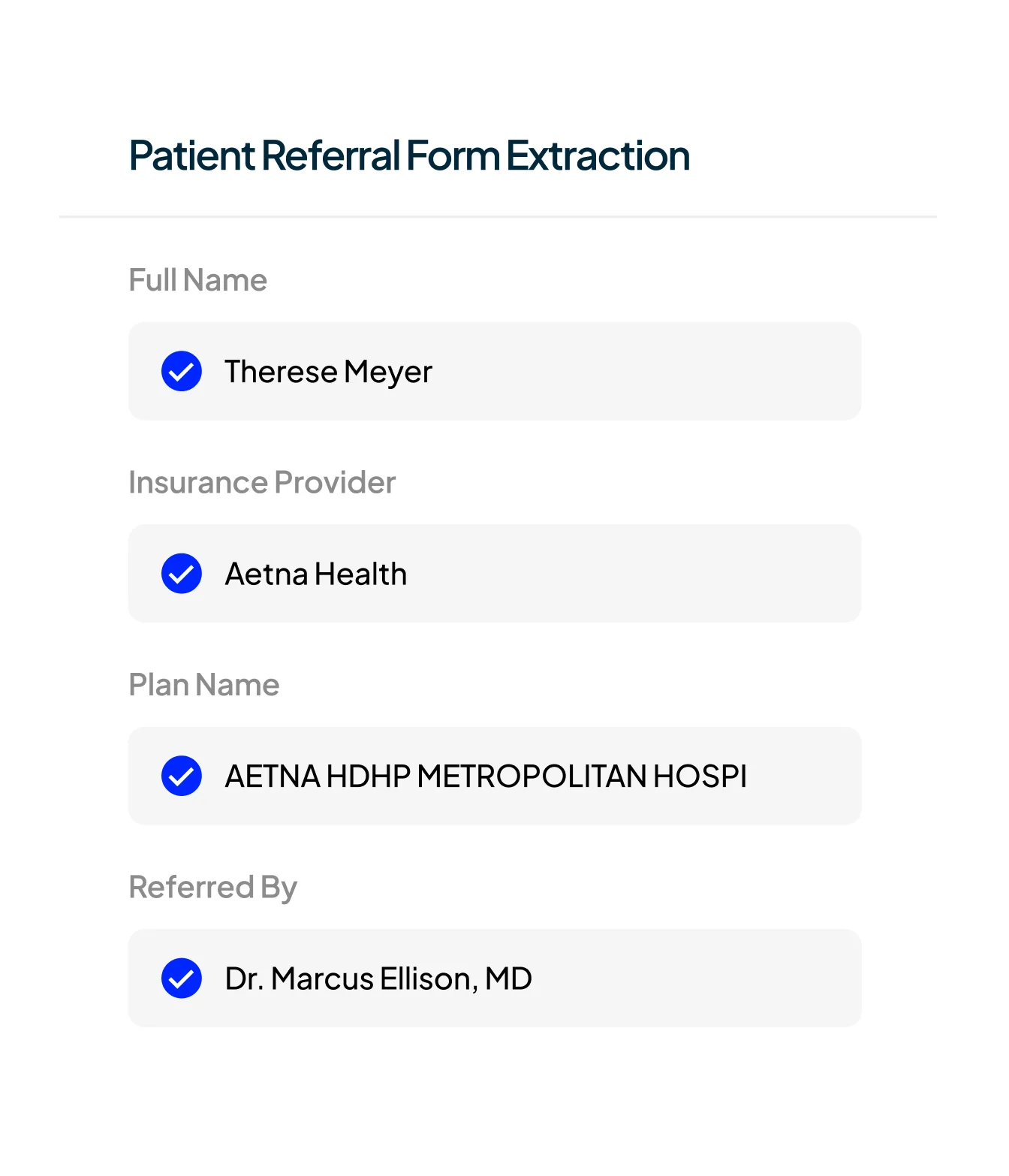
Mandolin instantly reads, interprets, and acts on referral forms, lab reports, and clinical notes — regardless of formatting or source. Using advanced multimodal AI, it extracts the right data points and intelligently routes each patient to the correct workflow, system, and care team — based on urgency, diagnosis, payer, and site-of-care logic.
Learn more
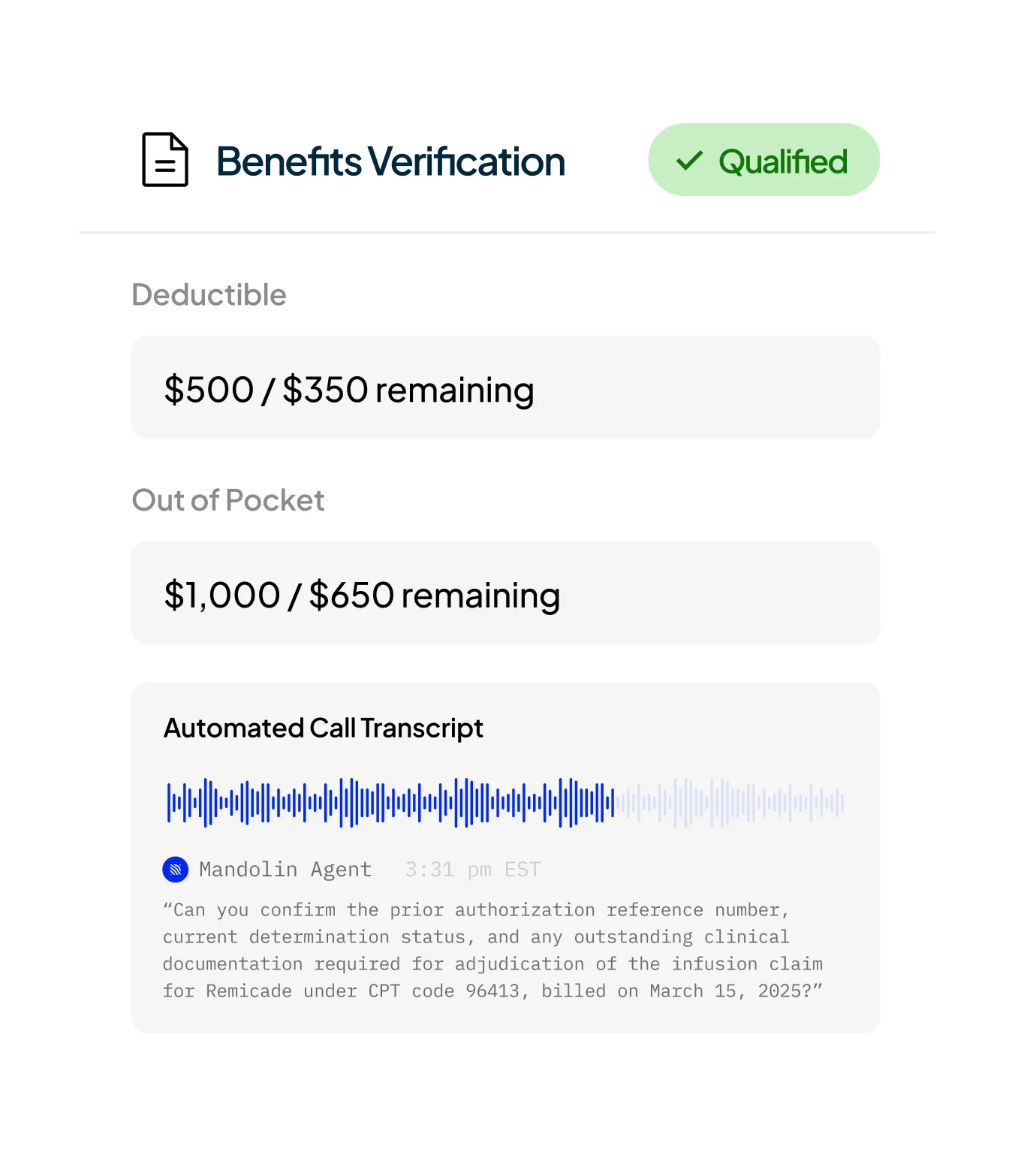
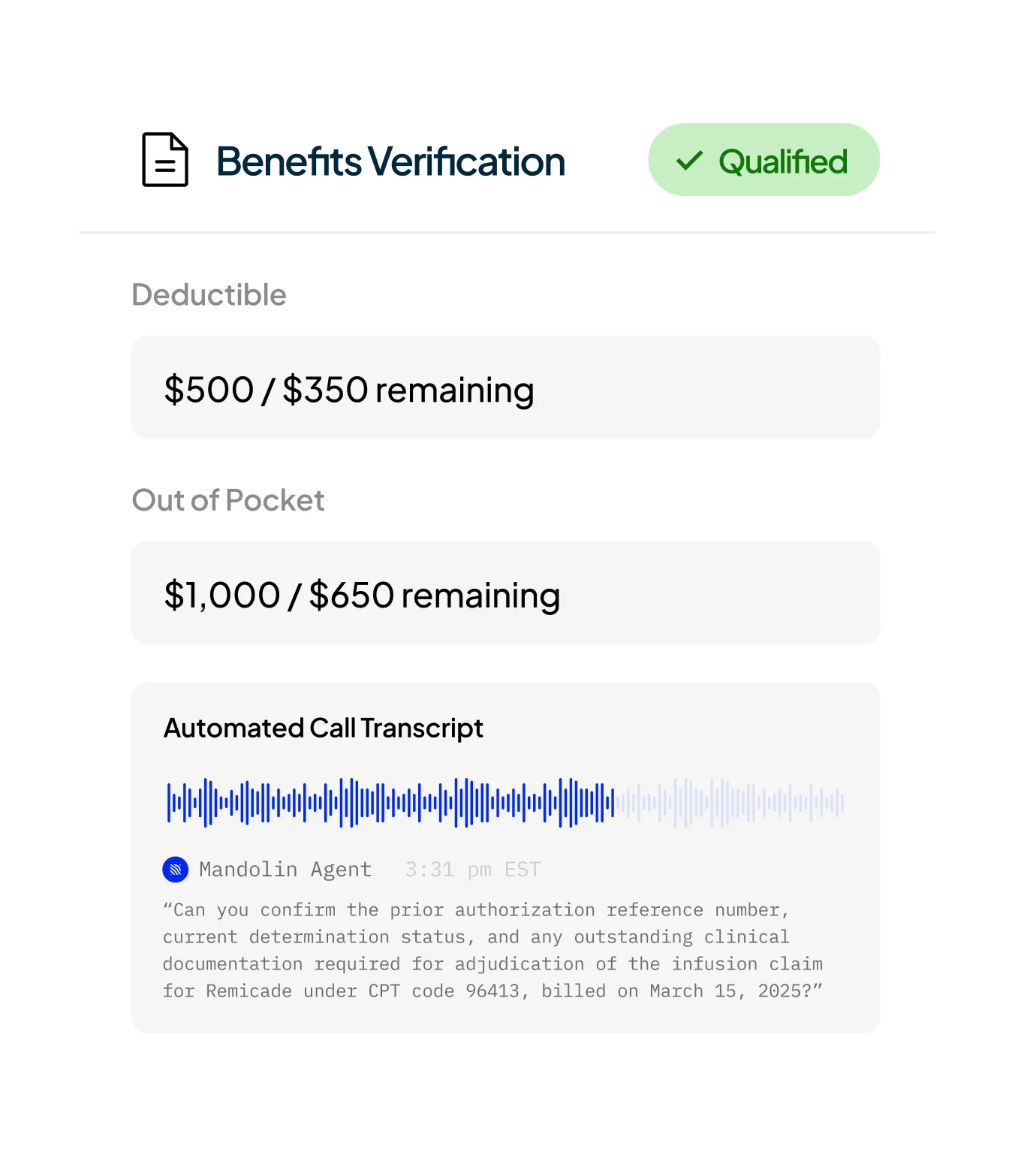
Mandolin performs full benefits investigations by navigating payer portals, extracting eligibility data, and making outbound calls — just like a trained back-office specialist.
The result: accurate coverage insights delivered at record speed, without manual effort.
Learn more
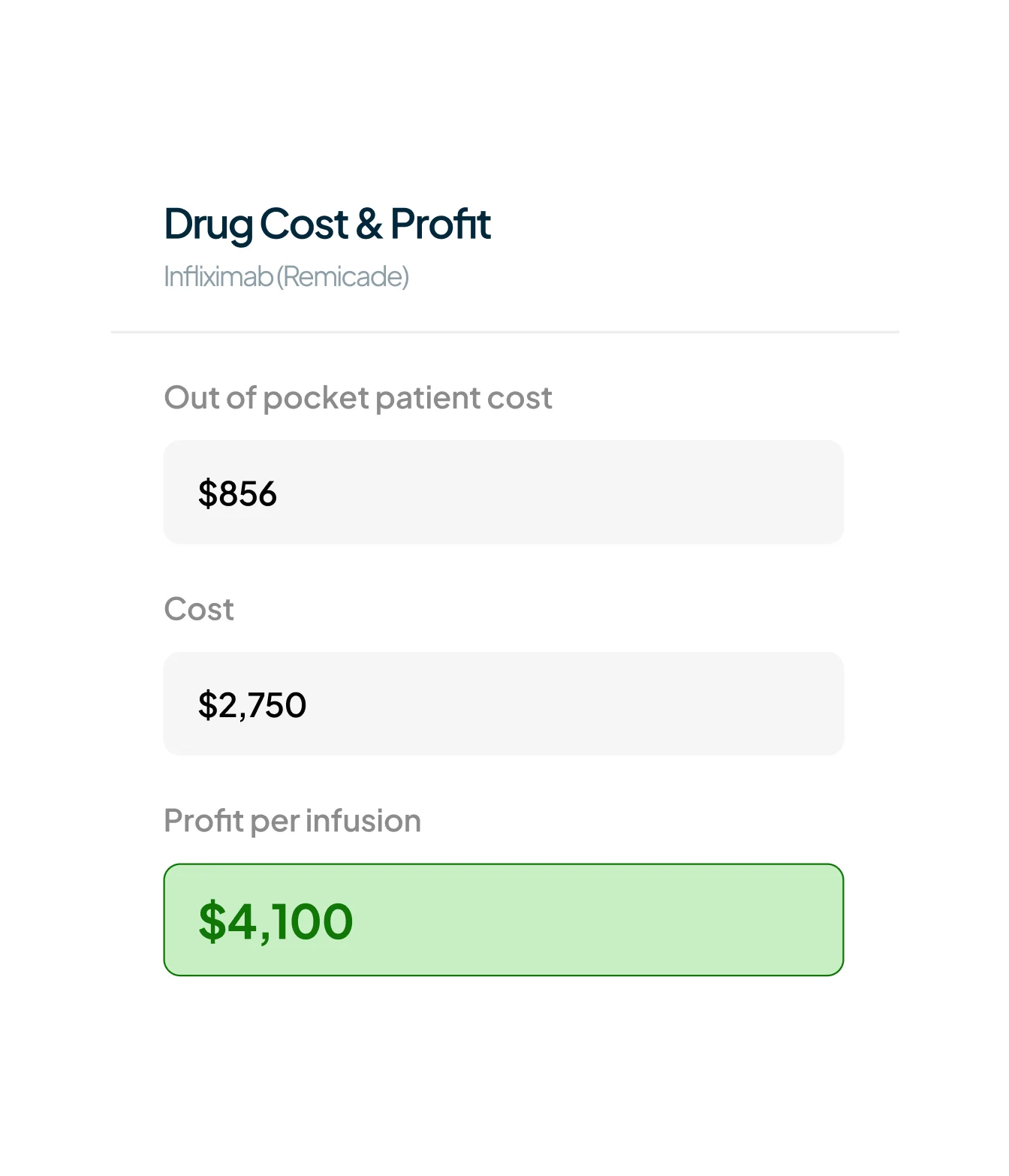
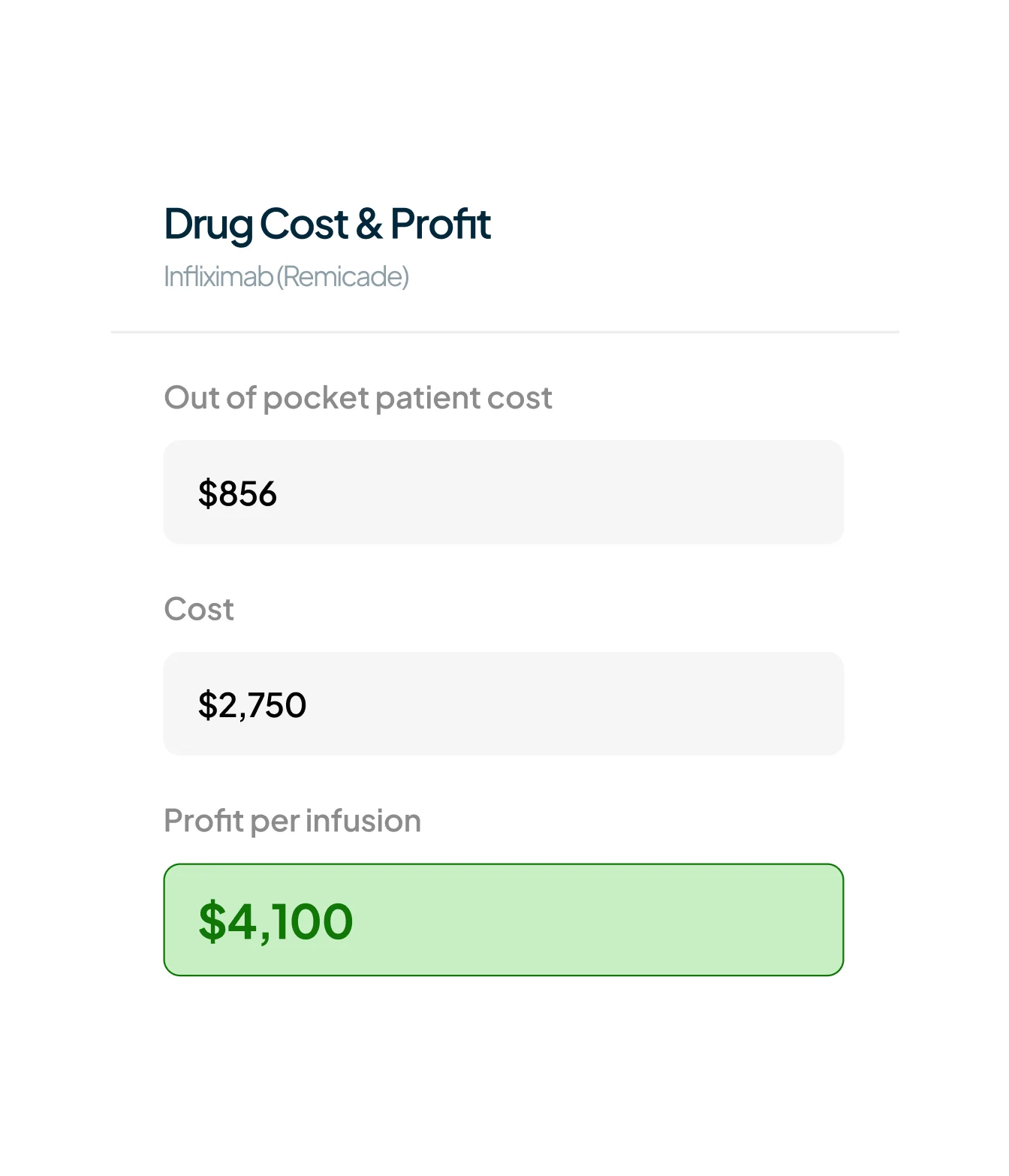
Calculates patient out-of-pocket costs with precision — factoring in real-time benefits, site-specific fee schedules, GPO and 340B pricing, and drug acquisition costs. Highlights the most profitable site of care for each drug while keeping patient affordability front and center. This enables smarter financial decisions at the point of intake, helping teams reduce friction, maximize margins, and improve patient access.
Learn more
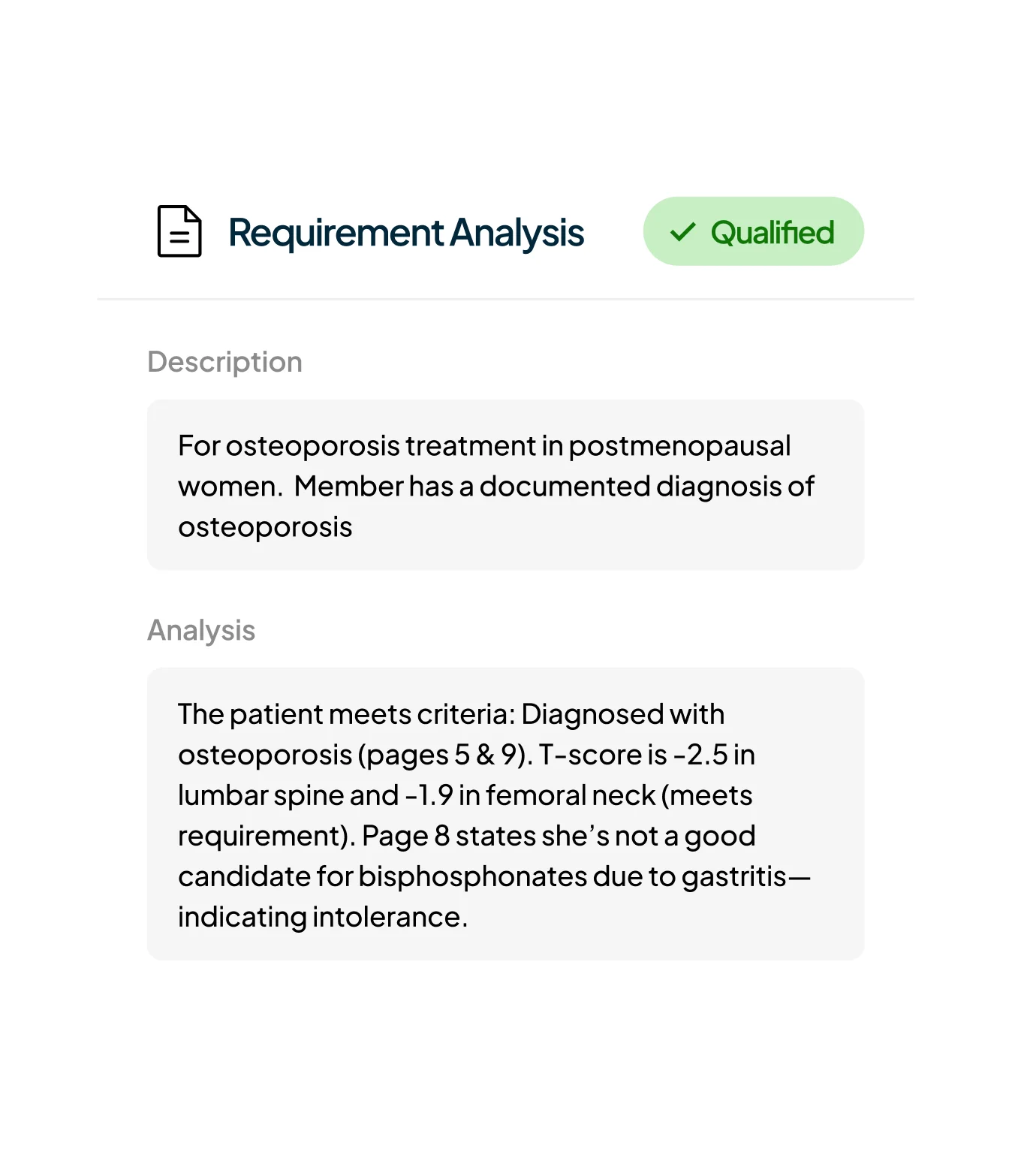
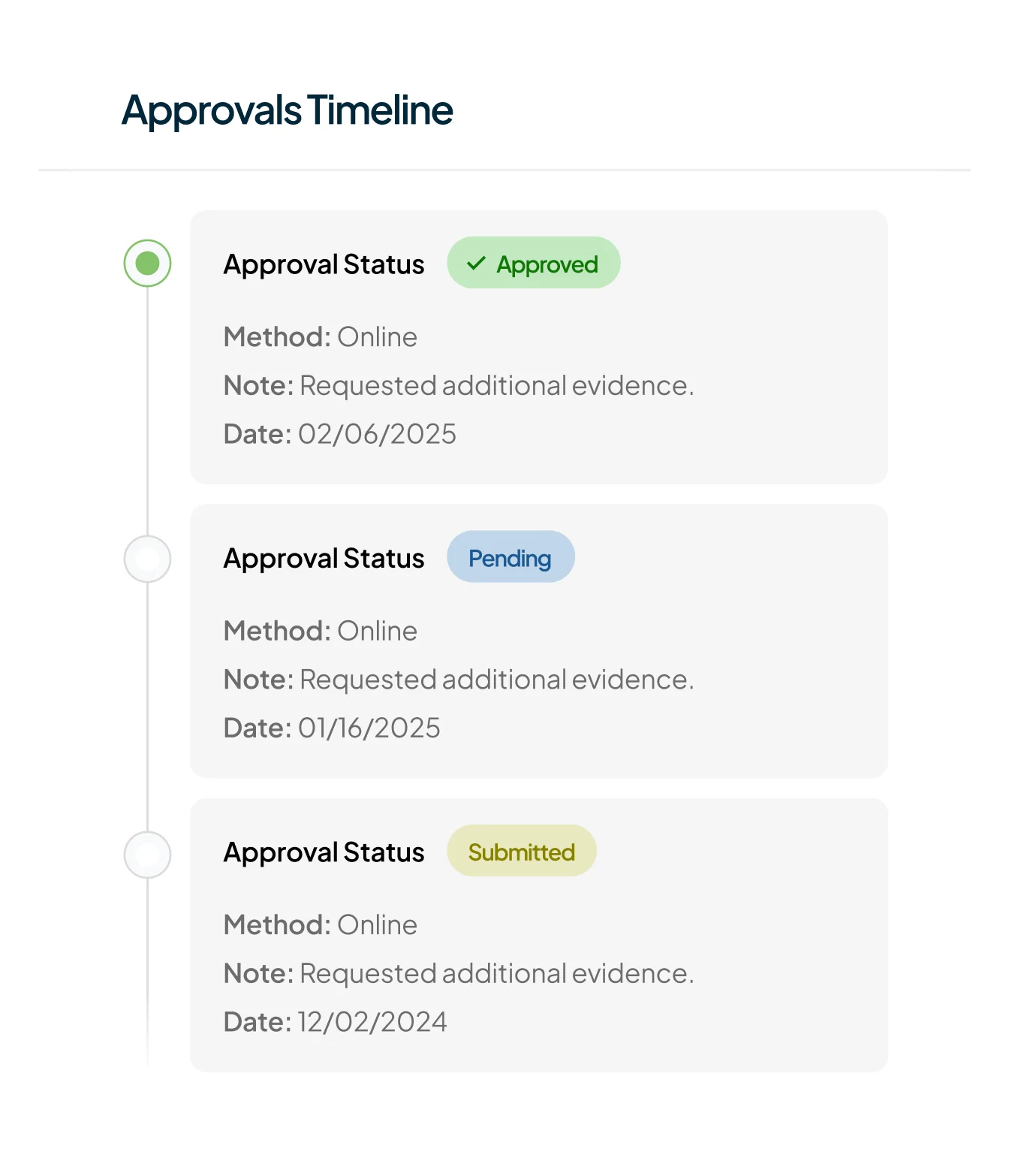
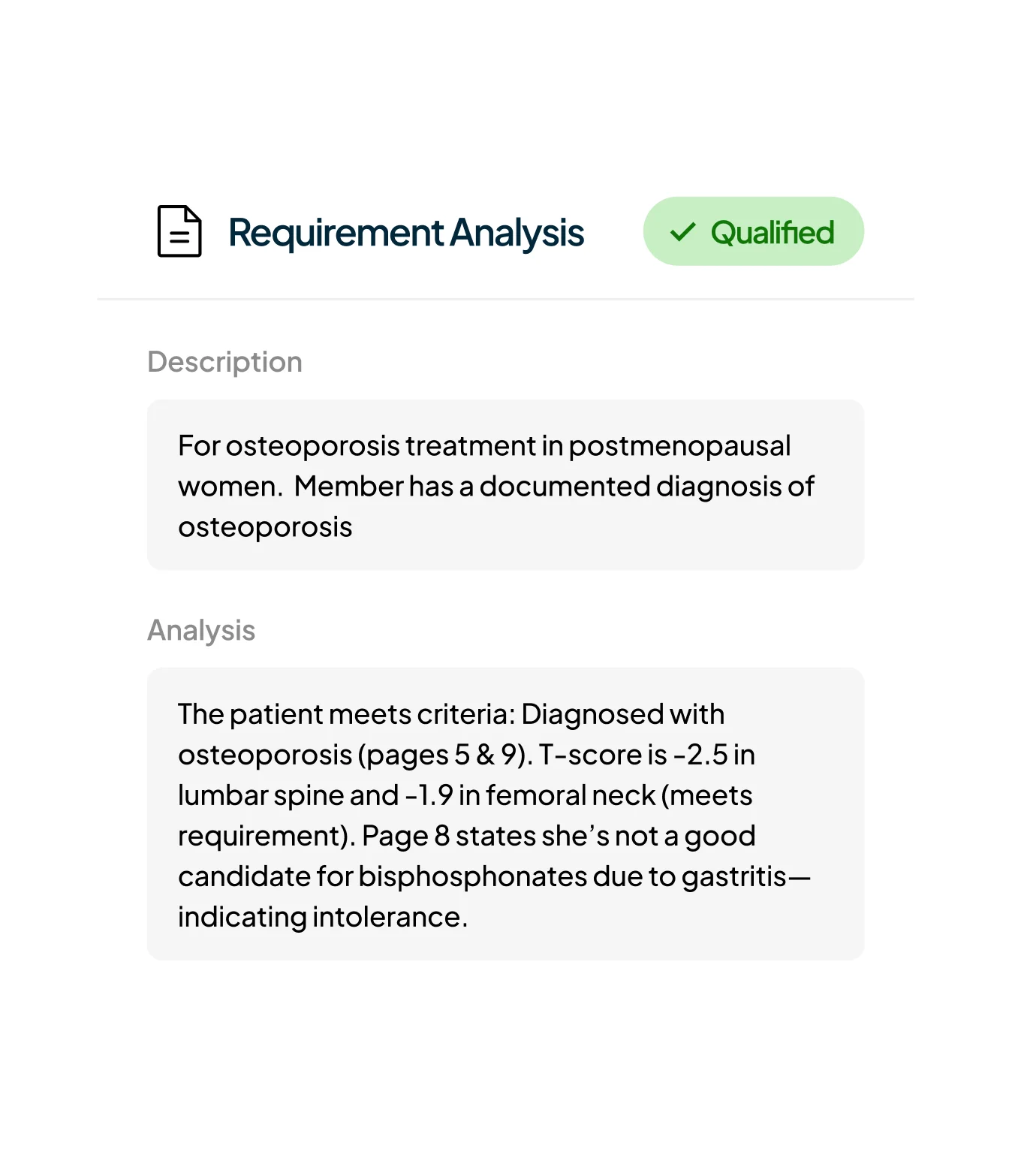
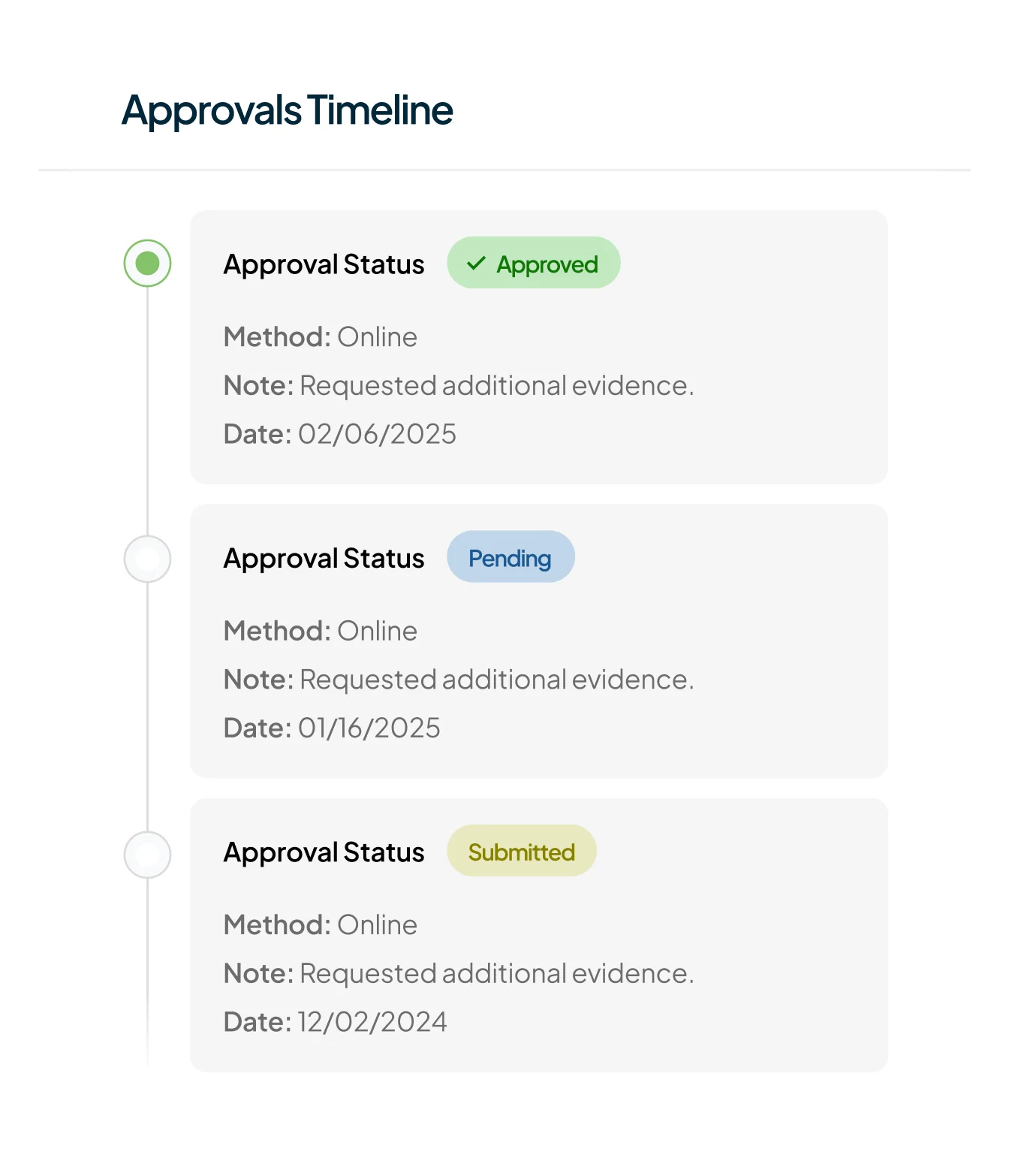
Connects across payer portals, sends required faxes, and follows up on status — automatically. Pulls in clinical documentation, reviews policy criteria, and prepares complete submissions that align with each payer’s rules. Every step — from chasing notes to tracking approvals — is handled behind the scenes.
Learn more
Tracks claim status automatically by making outbound payer calls and interpreting remits, so your team doesn’t have to spend hours chasing updates. When a denial is detected, the system assembles a draft appeal packet — pulling in payer-specific denial criteria, clinical documentation, and supporting notes. This helps teams respond faster and more accurately, accelerating revenue recovery and reducing the risk of missed appeal windows.
Learn more
Start Anywhere.
Scale When You’re Ready
No big rollout. No lock-in. Just value from day one. Whether it’s benefits verification, prior auths, or claims — Mandolin can plug into a single part of your process and deliver immediate results. When you’re ready, you can expand to other steps in the infusion lifecycle with the same AI infrastructure.

Scale without increasing headcount
Automates every back-office task, from data entry to payer calls.

AI That Builds Trust Over Time
Keep humans in the loop — your staff can review, guide, or take over tasks using custom-built tools designed around their workflows.
Works in Your Systems.
Just Like a Human Would.
Our Mandolin agent doesn’t need integrations or special setup. It logs into your existing portals, EHRs, and payer tools — completing work exactly like a trained staff member would. Except it’s faster, more reliable, and always on.

No Integration required
No HL7, no FHIR, no dev time. Just provision an account and go.

Works With Any System
Handles tasks inside EHRs, payer portals, and even spreadsheets.